
Caroline Williams
BTEC Level 6 Professional Diploma in Advanced Clinical and Sports Massage, Jing Advanced Clinical Massage school.
Background: Low back pain is the leading cause of disability worldwide and more research into viable, accessible treatments is urgently needed. The aim of this research is to assess the efficacy of massage and earthing (the transference of electrons from the earth into the body) in the treatment of chronic low back pain.
Method: 12 participants with chronic low back pain were recruited via social media to take part in the research. All participants had suffered from non-specific low back pain for over three months. The Bournemouth Back Pain questionnaire was used during an initial six-week control period and throughout the treatment period, thus establishing levels of low back pain before and after the intervention. Following the control period, participants were randomly assigned into two treatment groups: the grounded group (GRD, grounded sleeping, n = 6) or the sham grounded group (UGD, sh- am-grounded sleeping, n= 6). Both groups were given an identical looking earthing sleep mat and the UGD group’s sleep mat was ‘shammed’. Participants were asked to sleep using the mat every night during the intervention phase. All participants attended clinic to receive a course of six massage treatments, based on the Jing method of clinical massage, which included self-care guidance.
Results: The GRD group’s pain improved by an average of 38% compared to an average of 17% for the UGD group. Both Jing Advanced Clinical Massage and the combination of Jing Advanced Clinical Massage and earthing may help to significantly reduce CLBP.
Conclusion: This research sets out a compelling case for treating chronic low back pain with a combination of Jing Advanced Clinical Massage and earthing. Due to the small-scale nature of this research, further research on a larger scale is necessary.
Low back pain (LBP) is the number one cause of disability on a global level, with 540 million people affected at any one time (Hartvigsen et al., 2018). It is a growing problem due to the ageing population and the burden of LBP is set to increase (Buchbinder et al., 2018).
The current National Institute for Health and Care Excellence (NICE) guidelines on the management of LBP recommends manual therapies including massage as a non-invasive treatment approach, alongside exercise (Bern- stein et al., 2017). Earthing (which refers to bodily contact with the earth’s natural electrical charge) has also been proposed by Menigoz et al. (2020) as a potential treatment for pain.
This study intends to assess the efficacy of clinical massage using the Jing Method as described by Fairweather and Mari (2015) and earthing as interventions in the treatment of chronic low back pain through a double-blind ‘randomised trial.
It is estimated that between 5 – 10% of people that suffer from a period of acute LBP will develop chronic low back pain (CLBP), which is defined as pain lasting for more than three months (Meucci, et al., 2015).
The latest guidelines for treatment of CLBP recommend the use of the biopsychosocial approach which considers the biological, psychological and social factors which can all play a role in the persistence of pain (Foster et al., 2018).
This approach acknowledges that emotions play a role in pain, for example, depression and anxiety have long been associated with chronic pain syndromes (Diamond and Borenstein, 2006). Also, attitudes towards pain and catastrophising thoughts, especially during the acute phase can increase the chances of the pain persisting beyond three months. A person’s social circumstances can also impact their chances of developing CLBP and research has shown that lower education levels and socio-economic status are a strong predictor of prolonged pain and increased likelihood of pain becoming chronic (Fairweather and Mari, 2015:34-36; Diamond and Borenstein., 2006).
The biopsychosocial approach has shifted CLBP from being a medical problem to a ‘positive health’ perspective. The focus on self-management, exercise and psychological programs such as cognitive behaviour therapy alongside therapies such as massage is more successful than pharmaceutical or surgical management of CLBP and is now the recommended treatment modality (Buchbinder et al., 2018).
In one of the latest review papers on treatment recommendations for CLBP Forester et al (2018) state that UK guidelines endorse the use of complimentary treatment including massage. The same paper then goes onto to state that some guidelines recommend against the use of therapies such as massage. This suggests at the outset that the case both for and against massage as a treatment for CLBP is not clear-cut.
Despite this uncertainty, massage remains a popular treatment for those with LBP, accounting for up to one third of visits to a massage therapist in the US (Cherkin et al., 2009). The existing research into the efficacy of massage raises numerous problems including studies which employ too few massage treatments, lack of information on patient population and the heterogeneity of the research. These factors make it hard to compare studies and draw broad conclusions (Ernst, 1999).
As well as the general lack of published evaluations, the challenge with research is that massage is not a standardised treatment. There are many variables which potentially affect the outcome, including massage technique, duration, frequency of treatment, pressure used, and experience of the massage therapist (Furlan et al., 2015).
(Bervoets et al., 2015a) defines massage as ‘a systematic manipulation of the soft tissues of the body with rhythmical pressure and stroking to prevent, develop, maintain, rehabilitate, or augment physical function or relieve pain’. The most common relaxation massage techniques include effleurage, petrissage, friction, vibration, rocking and holding (Cherkin et al., 2009).
In 2009 Cherkin at al, conducted a study with the aim of determining if relaxation massage, using the techniques outlined above, is an effective treatment for LBP in terms of reduced pain and improved function. The research went on to compare the effectiveness of relaxation massage with focused structural massage to establish which was more effective.
The results showed massage to be a more effective therapy in comparison to ‘usual care’ for LBP with both decreased pain and improved function for those that received both types of massage therapy after 10 weeks of treatment. There was no significant difference in the treatment outcomes from the two different styles of massage (Cherkin et al., 2011).
In contrast to this research Furlan et al (2015) conducted a comprehensive review to assess the effects of massage therapy for people with non-specific LBP and found little evidence to support massage as an effective treatment for LBP. The review went on to state that massage improved pain and function outcomes in the short-term for sub-acute and CLBP but not in the long-term (Furlan et al., 2015).
There is also uncertainty on how massage therapy works to reduce pain and by which mechanism. Some believe a shift from sympathetic to parasympathetic response, mainly focusing on massage’s effect to the central nervous system. Biomedical changes are also posed as a mechanism for massage due to increased blood and lymph flow (Bervoets et al., 2015a).
Others believe its effectiveness could be down to spending time in a relaxed environment, the therapeutic experience of touch and focused attention on the self and increased body awareness (Cherkin et al., 2009.).
Despite the uncertainty around the efficacy of massage as a treatment for LBP, the current National Institute for Health and Care Excellence (NICE) guidelines on management of low back pain does recommend massage as a viable treatment option (Bernstein et al., 2017).
This study specifically investigates the effectiveness of the Jing protocol on CLBP. This is relevant to the current medical guidelines which view CLBP within a biopsychosocial model of pain. Therapists trained in the Jing method understand the importance of the biopsychosocial model of pain and address it through their consultation process, the specific techniques used and self-care advice given.
As part of the Jing Advanced Clinical Massage method, teaching participants self-care is an important element. In this study participants will receive two dedicated self-care sessions delivered via Zoom.
It has been shown that massage combined with self-care is a powerful combination for CLBP (Fairweather and Mari, 2015:177-194). Cherkin et al 2001, suggests that massage together with self-care could prove to be a very cost-effective solution to LBP. His research showed that while massage was better at reducing LBP levels in the short term, in the longer term the self-care educated group had comparable pain reduction as massage (Cherkin et al., 2001.).
Self-care by its very nature empowers people to take back control over their pain The traditional western ‘biomedical’ approach in which the doctor is paternalistic and holds the knowledge / power to ‘fix the problem’ is in direct opposition to an emphasis on self-management and empowerment. (Fairweather and Mari, 2015:177-194). It could well be the patients feeling of control over their pain that is the key to reducing it. This can be explained by having an internal locus of control or sense of agency around the pain. Research has shown that patients that believe that they can alter their own circumstance by their own actions have better outcomes when it comes to LBP (Fairweather and Mari, 2015:177-194; Coughlin et al., 2000).
Another key element of this study is looking at whether earthing can positively impact CLBP. A significant amount of research is emerging on the effects of direct physical contact with the surface of the earth in terms of its anti-inflammatory and antioxidant benefits. These effects have even been described as a form of ‘electric nutrition’ (Sinatra et al., 2017).
Over the last ten years, research has shown that significant healing benefits can be gained from the earth’s electrical charge and the transference of electrons from the earth into the body. This transference results in physiological changes that can improve sleep, reduce pain and inflammation, and improve blood flow (Sinatra et al., 2017; Chevalier, Brown and Hill, 2015).
The term ‘electron deficiency’ has been used to describe what happens when there is no direct skin contact with the earth due to wearing shoes with synthetic soles and therefore no natural supply of electrons. One theory is that this lost contact with the earth over time has led to a build-up of positive electrical charge and therefore imbalance in the body leading to dysfunction, disorder and disease (Menigoz et al., 2020).
It is thought that earthing works through its influence on the bioelectric nature of the body and the continuous molecular network that extends throughout the body. The same system-wide network that forms the basis of the meridian system in traditional Chinese medicine (Oschman 2009). This ‘living matrix’ facilitates the movement of electrons to where they are most needed so they can reach and neutralize free radicals that cause chronic inflammation. Oschman (2009) hypothesizes that electrons entering the body saturate the mitochondria and in turn increase the availability of the adenosine triphosphate that energise the cells involved in tissue repair.
Various studies have shown how earthing impacts inflammation and pain. Two studies were undertaken to assess the effect of earthing on recovery after eccentric muscle loading and delayed onset muscular soreness (DOMS). One of the studies was designed to assess inflammation markers (due to micro trauma in the muscle fibres) and pain scale differences between a group that were grounded (another term used to describe the process of earthing) after the eccentric exercise and a ‘sham grounded’ group. This research showed that grounded sleeping resulted in faster recovery and reduced muscle fibre damage and inflammation (Müller et al., 2019).
The second study on DOMS and muscle recovery, showed that earthing fol- lowing eccentric exercises, changed blood counts relating to inflammation and showed lower blood creatine kinase indicating reduced muscle damage (Chevalier, Brown and Hill, 2015).
To date there hasn’t been any specific research on the effects of earthing on CLBP. The existing research, mentioned above, as well as thermal imaging shows that the influx of the earth’s electrons has an anti-inflammatory effect on the body (Menigoz et al., 2020) which in turn may work to reduce pain.
Based on the findings of my literature review, I hypothesize that the Jing Advanced Clinical massage and self-care interventions will be effective in reducing CLBP at 13 weeks, and the group that receive the real earthing will receive additional benefits in terms of pain reduction.
Ethical approval was received for the following study from Jing Advanced Massage Training. A group of 12 participants with CLBP were recruited via social media (7 female and 5 male participants were recruited, all aged between 35– 80 years old). All participants gave written, informed consent. Two participants subsequently dropped out of the study before completion and their data has not been included in the results.
CLBP for the purposes of this trial was defined as pain that persists longer than three months and that is localised below the scapulae and above the cleft of the buttocks. Non specific indicates that no specific cause was detectable, such as, infection, neoplasm, metastasis, osteoporosis, rheumatoid arthritis, fracture, or inflammatory process (Heymans et al., 2004).
The inclusion criteria for the study also included participants scoring a minimum of three out of ten when asked to rate their average back pain levels.
The study had an ingroup control with participants completing the Bournemouth Back Pain questionnaire for 6 weeks prior to the commencement of treatment to establish level of back pain. The questionnaires were submitted weekly over the six-week period. All the participants agreed not to have any other massage or physical therapy for the duration of the study.
All participants attended clinic to receive a six-week course of massage therapy and self-care instruction based on the Jing Advanced Clinical Massage HFMAST protocols for low back pain (Fairweather and Mari, 2015).
See appendix for further details on the treatment protocol.
The participants were randomly assigned to the grounded group (GRD, grounded sleeping, n = 6) or the sham grounded group (UGD, sham-grounded sleeping, n= 6). Both groups were given an identical earthing sleep mat with the same usage instructions and were told to sleep using the mat every night during the intervention phase (7 weeks in total). The cords used for sh- am-grounding were modified so that they prevented connection to the earth (they maintained an open circuit). No difference could be seen between functioning grounding cords and sham-grounding cords. The earthing sleep mats and cords were provided by www.earthing.com.
Throughout the treatment phase, participants continued to fill in the Bournemouth Back Pain questionnaire weekly, with the last questionnaire completed 7 days after the final massage treatment and after 7 weeks of using either the real or sham earthing sleep mat.
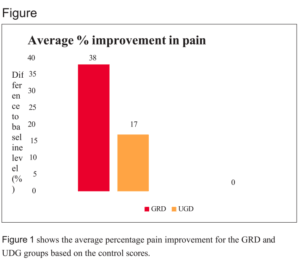
The GRD group’s pain improved by an average of 38% compared to an average of 17% for the UGD group. Overall, the GRD group had a higher decrease in their CLBP compared to the UGD group.
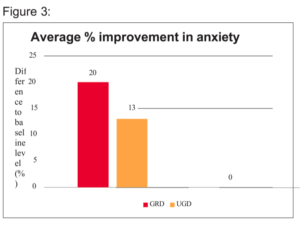
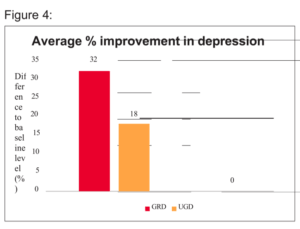
Figure 3 & 4 show the average percentage improvement for participants based on their control scores for anxiety and depression.
In line with the ‘biopsychosocial’ approach, as discussed in the introduction, it is known the ‘the issue is not always in the tissues’. Stress and raised cortisol levels lead to a prolonged ‘fight or flight’ response which can also lead to chronic pain. Both the GRD and UGD groups also benefited from a significant reduction in anxiety (GRD: 20% UGD:13%) and depression (GRD:32% UGD: 18%).
The main findings of this study are fourfold: (1) Both Jing Advanced Clinical Massage and the combination of Jing Advanced Clinical Massage and earthing may help to significantly decrease CLBP; (2) The combination of earthing and massage may have a greater impact at reducing CLBP than massage alone; (3) Both earthing and massage may help to reduce anxiety and depression; (4) The combination of earthing and massage may have a greater impact at reducing anxiety and depression than massage alone.
Due to the small-scale nature of the study there are certain limitations which need to be taken into consideration. Firstly, the participant population in this study was too small to draw broad, generalised conclusions, and rather it should be treated as a pilot study.
Secondly, the nature of CLBP means the condition can have periods of stability and periods of flare-up where pain increases, and this can also be true as healing takes place. As the body heals and rebalances pain can fluctuate sometimes getting worse before getting better.
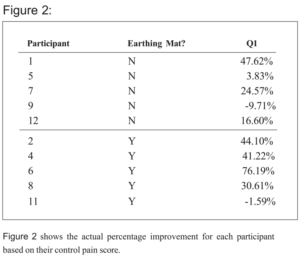
Within the sample 20% of participants did experience a flare-up during the study, which when dealing with such a small sample can have a large impact on the results. One example of this was ‘participant 11’ from the GRD group who was also suffering from shoulder pain at the outset of the study. The participant’s shoulder pain resolved whilst her back pain increased, but if the study had been longer, she may have also experienced improvements in her back pain.
Participant 9, in the UGD, group also had a flare in pain during the intervention phase, but by week 13 had a reduction in pain compared to baseline. The higher pain scores during the flare period meant that the overall improvement was not reflected in the average percentage improvement pain score for that participant.
A key part of Jing Advanced Clinical massage is the ‘fix in six’ approach (Fairweather and Mari, 2015). The recommendation is that the client receives six treatments to achieve a reduction in their pain. In this study the intervention phase was indeed 6 weeks. Four ‘hands on’ massage treatments were given as well as two self-care sessions taught over Zoom. The trend for both the GRD and UGD groups showed pain decreasing over time. It would have been in- interesting to continue the weekly ‘hands-on’ treatments for another few weeks to assess whether this trend continued.
It would be interesting to continue the follow-up with participants to assess the long-term benefit of a course of massage and earthing. Furlan et al (2015) in his review looking at massage therapy for LBP, concluded that massage therapy improved pain in the short term but not in the long term. It would be beneficial to know the long-term effects of the intervention and whether this differed between the GRD and UGD groups.
It could be argued that two interventions (in this case massage and earthing) are bound to lead to better results due to the expectation that two interventions are better than one at reducing pain. However, due to the double-blind nature of this study all participants benefitted from the placebo effect of two interventions. The results clearly show without bias that the GRD group had greater pain reduction than the UGD group.
For this combination of treatment, the most cost-effective solution for CLBP would be a six-week course of clinical massage and longer-term use of an earthing device or daily outdoor barefoot earthing for a minimum of 30 minutes per day. Interestingly, the cost of earthing devices starts at around £40 – £50, which is less than a year’s supply of medication prescription charges in the UK (£108.10 for 12 months). The latest recommendations for the prescription of medication for CLBP recommends short-term use of non-steroidal anti-inflammatory drugs and weak opioids. Most guidelines also recommend antidepressants, where necessary, as a treatment for CLBP (Oliveira et al., 2018).
The results of this pilot study indicate that both massage and earthing and ideally the combination of both may work to reduce CLBP. What is missing is an understanding of the mechanisms of how both interventions work to reduce CLBP.
From considering the biopsychosocial model, CLBP can have biological, psychological and social origins. The Jing method treats not only the biological and addresses the ‘issues in the tissues’ but also the psychological by activating the parasympathetic nervous system during treatment thus lowering cortisol. It’s also key to consider the therapeutic alliance established between therapist and patient. A positive therapeutic alliance is central to the Jing method and according to research by Ferreira et al (2013) is associated with significantly better outcomes in LBP.
Earthing also works to bring homeostasis to the body through its effect on different systems. Previous research has shown earthing to positively impact inflammation, stress, sleep, energy, blood flow as well as pain (Menigoz et al., 2020). In this sense perhaps earthing and massage together work on the many different levels required to treat complex chronic pain.
One of the reasons this research did not have a third group of participants just receiving earthing as an intervention was because the research wasn’t about positioning earthing against massage to see which was the most effective. The research is about taking nature’s healing modalities and showing for the first time, that together they are a potent combination in overcoming the all too common and complex problem of chronic pain.
Ochman et al (2018) noted: “The world is crying in pain. The world has a solution. The planet itself, Nature’s original painkiller”. In the same way that earthing is a universally and timelessly available healer, the instinctive urge to touch someone in discomfort to help ease that pain is “one of the deepest behaviours that define us and our kindred mammals.” (Fairweather and Mari,2015). Both the electrons from the earth and informed touch are powerful healing solutions – and more research is necessary into how they can work to reduce chronic pain.
In conclusion the results suggest that the combination of Jing Advanced Clinical Massage and earthing may lead to clinically significant improvements for CLBP. The combination of both interventions had better results in terms of pain reduction than massage treatment alone.
Therefore, there is a compelling case for earthing to be included as a key self-care recommendation given to patients with CLBP alongside massage therapy. Due to the small-scale nature of this research, further research on a larger scale is necessary.
Bervoets, D.C., Luijsterburg, P.A.J., Alessie, J.J.N., Buijs, M.J. and Verhagen, A.P.2015a. Massage therapy has short-term benefits for people with common musculoskeletal disorders compared to no treatment: A systematic review. Journal of Physiotherapy 61(3), pp. 106–116. doi: 10.1016/j.jphys.2015.05.018.
Bervoets, D.C., Luijsterburg, P.A.J., Alessie, J.J.N., Buijs, M.J. and Verhagen, A.P.
2015b. Massage therapy has short-term benefits for people with common musculoskeletal disorders compared to no treatment: A systematic review. Journal of Physiotherapy 61(3), pp. 106–116. doi: 10.1016/j.jphys.2015.05.018.
Buchbinder, R. et al. 2018. Low back pain: a call for action. The Lancet 391(10137), pp. 2384–2388. doi: 10.1016/S0140-6736(18)30488-4.
Chan, Y.-C., Wang, T.-J., Chang, C.-C., Chen, L.-C., Chu, Y., Lin, S.-P. and Chang, S.-T. [no date]. Short-term effects of self-massage combined with home exercise on pain, daily activity, and autonomic function in patients with myofascial pain
Cherkin, D.C. et al. 2011. A Comparison of the Effects of 2 Types of Massage and Usual Care on Chronic Low Back Pain A Randomized, Controlled Trial. Available at: www.annals.org.
Cherkin, D.C., Eisenberg, D., Sherman, K.J., Barlow, W., Kaptchuk, T.J., Street, J and Deyo, R.A. 2001. Randomized Trial Comparing Traditional Chinese Medical Acupuncture, Therapeutic Massage, and Self-care Education for Chronic Low Back Pain. Available at: https://jamanetwork.com/.
Cherkin, D.C., Sherman, K.J., Kahn, J., Erro, J.H., Deyo, R.A., Haneuse, S.J. and Cook, A.J. 2009. Effectiveness of focused structural massage and relaxation massage for chronic low back pain: Protocol for a randomized controlled trial. Trials 10. doi: 10.1186/1745-6215-10-96.
Chevalier, G., Brown, R. and Hill, M. 2015. Grounding after moderate eccentric contractions reduces muscle damage. Open Access Journal of Sports Medicine, p.305.doi: 10.2147/oajsm87970
Chevalier, G., Patel, S., Weiss, L., Chopra, D. and Mills, P.J. 2019a. The Effects of Grounding (Earthing) on Bodyworkers’ Pain and Overall Quality of Life:
A Randomized Controlled Trial. Explore 15(3), pp. 181–190. doi: 10.1016/j.explore.2018.10.001.
Chou, R., Qaseem, A., Snow, V., Casey, D., Thomas, ; J, Shekelle, P. and Owens,
D.K. 2007. Diagnosis and Treatment of Low Back Pain: A Joint Clinical Practice Guideline from the American College of Physicians and the American Pain Society. Available at: www.annals.org.
Cottrell, M.A. and Russell, T.G. 2020. Telehealth for musculoskeletal phys-
iotherapy. Musculoskeletal Science and Practice 48. doi: 10.1016/j.msk-
sp.2020.102193.
Coughlin, A.M., Badura, A.S., Fleischer, T.D. and Guck, T.P. 2000. Multidisciplinary treatment of chronic pain patients: Its efficacy in changing patient locus of control. Archives of Physical Medicine and Rehabilitation 81(6), pp. 739–740. doi: 10.1053/apmr.2000.5586.
Dagenais, S., Tricco, A.C. and Haldeman, S. 2010. Synthesis of recommendations for the assessment and management of low back pain from recent clinical practice guidelines. Spine Journal 10(6), pp. 514–529. doi: 10.1016/j.spinee.2010.03.032.
Dario, A.B. et al. 2017. Effectiveness of telehealth-based interventions in the management of non-specific low back pain: a systematic review with meta-analysis. Spine Journal 17(9), pp. 1342–1351. doi:
Diamond, S. and Borenstein, D. 2006. Chronic low back pain in a working-age adult. Best Practice and Research: Clinical Rheumatology 20(4), pp. 707–720. doi: 10.1016/j.berh.2006.04.002
Ernst, E. 1999. Massage Therapy for Low Back Pain: A Systematic Review.
Ferreira, P.H., Ferreira, M.L., Maher, C.G., Retshauge, K.M., Latimer, J., Adams, R.D. 2013. The therapeutic alliance between clinicians and patients predicts outcomes in chronic low back pain. Physical Therapy, Volume 93, pp.470 – 478.
Foster, N.E. et al. 2018. Prevention and treatment of low back pain: evidence, challenges, and promising directions. The Lancet 391(10137), pp. 2368–2383. doi: 10.1016/S0140-6736(18)30489-6.
Furlan, A.D., Giraldo, M., Baskwill, A., Irvin, E. and Imamura, M. 2015. Massage for low-back pain. Cochrane Database of Systematic Reviews 2017(12). doi: 10.1002/14651858.CD001929.pub3.
Hartvigsen, J. et al. 2018. What low back pain is and why we need to pay attention. The Lancet 391(10137), pp. 2356–2367. doi: 10.1016/S0140-6736(18)30480-X.
Heymans, M.W., van Tulder, M.W., Esmail, R., Bombardier, C. and Koes, B.W. 2004. Back Schools for Nonspecific Low Back Pain A Systematic Review Within the Framework of the Cochrane Collaboration Back Review Group.
Hoy, D. et al. 2012. A systematic review of the global prevalence of low back pain. Arthritis and Rheumatism 64(6), pp. 2028–2037. doi: 10.1002/art.34347.
Koes, B.W., van Tulder, M.W. and Thomas, S. 2006. Clinical review Diagnosis and treatment of low back pain.
Menigoz, W., Latz, T.T., Ely, R.A., Kamei, C., Melvin, G. and Sinatra, D. 2020. Integrative and lifestyle medicine strategies should include Earthing (grounding): Review of research evidence and clinical observations. Explore 16(3), pp.
152–160. doi: 10.1016/j.explore.2019.10.005.
Meucci, R.D., Fassa, A.G. and Xavier Faria, N.M. 2015b. Prevalence of chronic low back pain: Systematic review. Revista de Saude Publica 49. doi: 10.1590/S0034-8910.2015049005874.
Müller, E., Pröller, P., Ferreira-Briza, F., Aglas, L. and Stöggl, T. 2019. Effectiveness of grounded sleeping on recovery after intensive eccentric muscle loading. Frontiers in Physiology 10( JAN). doi: 10.3389/fphys.2019.00035.
NICE guideline [NG59] November 2016 Low back pain and sciatica in over 16s: assessment and management. www.nice.org.uk/guidance/NG59/chapter/Recommendations#assessment-of-low-back-pain-and-sciatica. Accessed 01.08.21
Oliveira, C.B. et al. 2018. Clinical practice guidelines for the management of non-specific low back pain in primary care: an updated overview. European Spine Journal 27(11), pp. 2791–2803. doi: 10.1007/s00586-018-5673-2.
Oschman, J.L. 2009. Charge transfer in the living matrix. Journal of Bodywork and Movement Therapies 13(3), pp. 215–228. doi: 10.1016/j.jbmt.2008.06.005. Oschman, J.L., Sinatra, S.T., Chevalier, G. and Martin Zucker [2018]. Earth – The Original Painkiller. TOWNSENDLETTER.COM
Patrick, N., Emanski, E. and Knaub, M.A. 2014. Acute and chronic low backpain. Medical Clinics of North America 98(4), pp. 777–789. doi: 10.1016/j.mcna.2014.03.005.
Petrozzi, M.J., Spencer, G. and Mackey, M.G. [no date]. Disruptive Impacts of Living With Chronic Low Back Pain and Experience of Psychologically Informed Physical Therapy-A Qualitative Process Evaluation of a Randomised Control Trial. Available at: https://orcid.org/0000-0001-7118-0270.
Sinatra, S.T., Oschman, J.L., Chevalier, G. and Sinatra, D. 2017. Nutrition 8
ALTERNATIVE THERAPIES.
Sokal, K. and Sokal, P. 2012. Earthing the human organism influences bioelectrical processes. Journal of Alternative and Complementary Medicine 18(3), pp.229–234. doi: 10.1089/acm.2010.0683.